RAS 단백질: 파악하기 어려운 표적?
인간 암의 약 20%가 최소 한 가지 RAS 돌연변이(K-RAS, H-RAS, N-RAS)와 관련이 있으며 결과적으로 RAS는 인간 암에서 가장 자주 변이가 발생하는 유전자계입니다. 세포 원형질 막에 위치한 RAS 단백질은 세포 성장 신호를 보내는 분자 스위치 역할을 합니다. 그러나 RAS 단백질은 돌연변이를 통해 지속적인 활성 상태를 유지하고 성장 신호를 무분별하게 전송하며 그에 따라 비정상적인 세포 증식과 암 발병을 초래합니다.
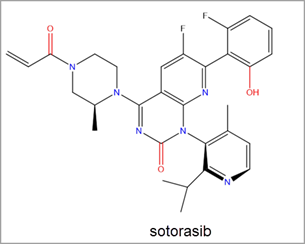
RAS 단백질은 이러한 다산성에도 불구하고 뚜렷한 관련 연구가 부족한 것이 사실입니다. 암 치료와 관련된 RAS 억제제 연구가 30년 넘게 진행되었지만 RAS 단백질은 발견하기 힘든 억제 전위로 인해 "약물 개발이 불가능"하다는 결론을 얻었으며 최근까지도 그렇게 인식되고 있습니다. 올해 초 FDA는 폐암 치료제로 소토라십(Amgen 개발, 상품명 Lumakras™)을 승인했으며 이는 치료제로 승인 받은 최초의 RAS 억제제입니다.
소토라십 승인은 RAS 억제 연구에 있어 유의미한 진일보로, 더 많은 RAS 억제제의 발견을 위한 연구 개발 노력이 증가하고 있습니다. 이 글에서는 RAS 단백질 연구 분야의 공백이 어떻게 해소되고 있는지 알아봅니다. 과거 약물 개발이 불가능한 것으로 알려졌던 표적이 이제 유망한 암 치료제로 떠오르고 있습니다.
K-RAS: RAS 유전자의 가장 일반적인 돌연변이
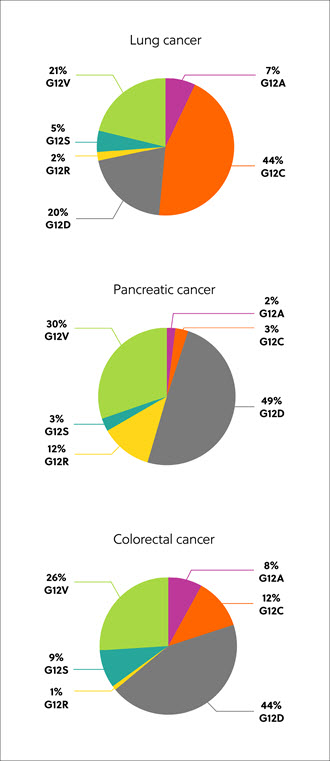
단백질의 RAS 유전자 코드는 네 가지 동형 단백질(K-RAS4A, K-RAS4B, N-RAS, H-RAS)에 존재합니다. 돌연변이된 RAS 동형 단백질, 코돈 및 아미노산 치환은 조직과 암 유형에 따라 다르지만 가장 일반적인 돌연변이는 K-RAS 동형 단백질에서 나타나며 약 22%의 RAS 돌연변이 암에서 발견됩니다. K-RAS 돌연변이의 80%는 시스테인(G12C, 14%), 아스파르트산(G12D, 36%), 발린(G12V, 23%)을 포함하여 글리신에서 다른 잔기까지 아미노산 위치 12에서 발생합니다(그림 1).1
암 치료 후보 약물로써의 RAS 단백질 발견
RAS 억제제는 X선 결정학으로 식별할 수 있습니다. 이 방법을 사용하면 RAS 단백질 구조를 검사하여 저분자가 인간 암 세포 내에서 점유하는 잠재적인 결합 포켓을 발견할 수 있습니다. 이러한 접근 방식, 즉 구조 기반 약물 설계는 특정 포켓 내에서 잠재적으로 결합될 수 있는 수백 가지 화학 물질을 발견할 수 있습니다. 잠재적인 RAS 억제제는 일반적으로 활성, 선별성을 강화하고 독성을 줄이기 위해 다양한 작용기로 약간 수정된 집적계로 구성됩니다. 그 결과, 인간 암 임상 시험에서 평가할 수 있도록 보다 세부적으로 분석, 강화 및 테스트할 수 있는 선도 화합물이 생성됩니다.
RAS 억제제와 관련된 최신 동향을 세부적으로 파악하기 위해 CAS Content Collection™에서 RAS 억제제와 관련된 특허 및 간행물을 검토했습니다. 분석 결과, 직접 RAS 억제 분야에서의 치료 또는 약리학적 역할과 관련된 26,958가지 화학 물질이 확인되었습니다. 이 분야의 화학 물질과 특허 건수는 매년 증가하고 있으며 이는 RAS 억제제 발견을 위한 연구 노력과 관심이 계속 늘어나고 있다는 사실을 뒷받침합니다(그림 2).

최근 FDA의 Amgen 소토라십 승인은 RAS 억제제 발견을 위한 연구 노력을 크게 증가시켰습니다. 소토라십은 Switch-II 포켓을 통한 KRAS G12C의 공유 결합 억제제로, 인간 암 치료와 KRAS G12C 돌연변이 비소세포폐암(NSCLC) 치료 용도로 승인을 받은 최초의 KRAS 억제제입니다(그림 3).2
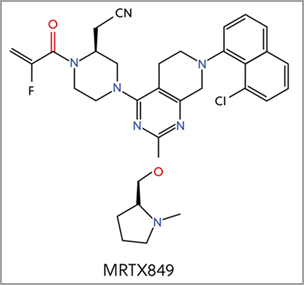
현재 다른 네 가지 KRAS-G12C 억제제도 추가 임상 시험 단계에 있으며 소토라십과 핵심 구조가 유사한 MRTX849를 예로 들 수 있습니다(그림 4)2. 작용기마다 Switch II 포켓의 주요 요소에 대한 결합 메커니즘이 다릅니다. FDA는 2021년 6월 MRTX849를 KRAS G12C 양성 NSCLC에 대한 혁신적인 치료법으로 지정했습니다.
계속되는 여정: 직접 RAS 억제제 표적의 다양성 확대
분자 결합 RAS가 계속 발견되면서 RAS 동형 단백질과 RAS 단백질의 표면 또한 잠재적인 저분자 표적으로 확인되고 있습니다.
돌연변이형 RAS 동형 단백질, 코돈 및 아미노산 치환은 조직과 암 유형에 따라 다르므로 현재 G12C 억제제에서 암 치료 범위를 넓히기 위해서는 다양한 접근법이 필요합니다. 앞으로 G12D, G12V와 같이 억제제의 표적이 될 수 있는 아미노산의 종류도 늘어나 보다 많은 유형의 암을 치료할 수 있을 것으로 기대되고 있습니다.
RAS 억제에 대한 본격적인 연구는 이미 시작되었습니다. 저분자 표적의 RAS 종양 단백질 구조와 결합 포켓 구성을 보다 정확하게 이해함으로써 새로운 RAS 억제제를 개발하고 RAS 돌연변이형 암에서 최적의 효능을 발휘하도록 기능을 개발하고 개선할 수 있습니다.
CAS 정식 보고서를 통해 RAS 표적 연구를 위한 지속적인 노력을 확인해 보세요. 화학 구조와 관련한 현재의 RAS 억제제에 대한 동향 개요와 미래 기회를 좀더 자세히 파악할 수 있습니다.
참조문헌
1. H. Chen 및 그 외, KRAS를 직접 표적으로 하는 저분자 억제제 항암 치료법(Small-molecule inhibitors directly targeting KRAS as anticancer therapeutics). J. Med. Chem. 63 (2020) 11404–14424. doi: 10.1021/acs.jmedchem.0c01312.
2. L. Goebel 및 그 외, KRASG12C 억제제 임상 시험의 짧은 역사(KRASG12C inhibitors in clinical trials: a short historical perspective). RSC. Med. Chem. 11 (2020) 760. doi: 10.1039/d0md00096e.